Acetylcholine (ACh) stands as one of the most vital neurotransmitters in the human body. It plays fundamental roles in muscle contraction, autonomic nervous system regulation, and cognitive functions.
The interplay between ACh and steroid hormones such as progesterone, estradiol, pregnenolone, DHEA, and vitamin D shapes complex neuroendocrine and metabolic pathways critical to health.
This article explores this neurotransmitter’s biosynthesis, its modulation by steroids, its clinical importance, and how factors like vagus nerve stimulation, glucose metabolism, and pantothenic acid influence its function.
Acetylcholine Production in the Body
ACh is synthesized predominantly in cholinergic neurons by the enzyme choline acetyltransferase (ChAT), which catalyzes the transfer of an acetyl group from acetyl-Coenzyme A (acetyl-CoA) to choline. This reaction occurs mainly in the nerve terminals. The availability of choline, sourced from dietary intake or recycling following breakdown, is a rate-limiting step in synthesis. Choline crosses the blood-brain barrier through sodium-dependent uptake channels, and nerve terminals in the central and peripheral nervous systems take it up.
Mitochondria generate acetyl-CoA from glucose metabolism—an essential step that directly links energy availability to neurotransmitter production. The vesicular acetylcholine transporter (VAChT) then packages the newly formed ACh into synaptic vesicles. A nerve impulse triggers calcium influx, releasing ACh into the synaptic cleft, where it binds to nicotinic and muscarinic receptors on post-synaptic cells. Acetylcholinesterase rapidly terminates its action by breaking it down into acetate and choline for recycling.
This complex synthesis and release mechanism ensures precise regulation of cholinergic signaling essential for motor control, cognitive processing, and autonomic functions like heart rate and digestion.
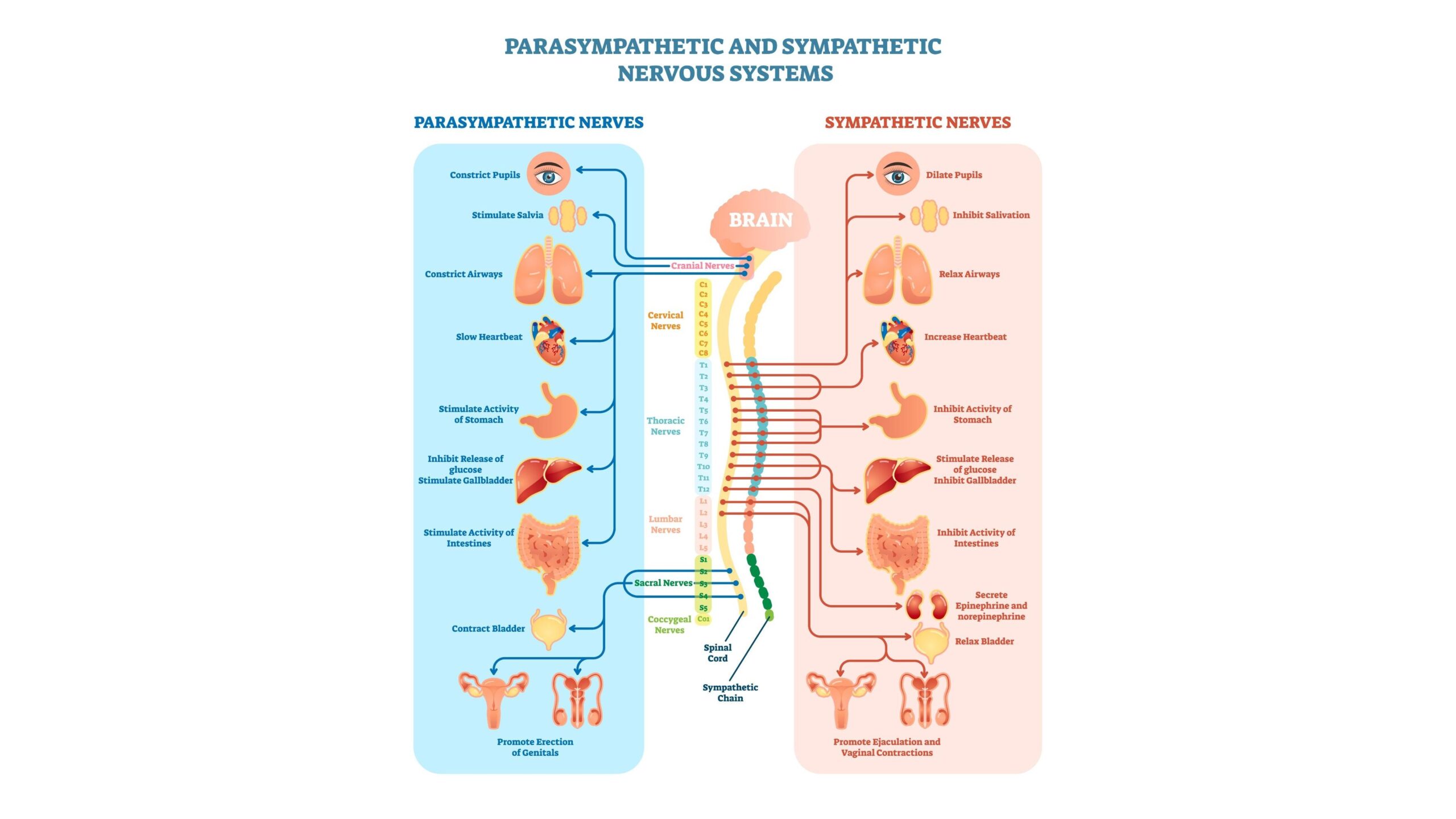
Acetylcholine’s Role in the Autonomic Nervous System (ANS)
Primarily serving as the principal neurotransmitter of the parasympathetic nervous system, ACh mediates the “rest-and-digest” responses essential for homeostasis. The vagus nerve, one of the longest cranial nerves, uses this messenger extensively to modulate cardiac function, gastrointestinal motility, and anti-inflammatory pathways.
Vagus nerve stimulation elevates release, enhancing parasympathetic tone and promoting beneficial effects such as reduced heart rate, improved gut secretion, and systemic anti-inflammatory actions. This has therapeutic applications in conditions ranging from epilepsy to inflammatory diseases.
Steroidal Hormones Modulating Acetylcholine Function
Estradiol, progesterone, pregnenolone, DHEA, and vitamin D modulate this neurotransmission through several mechanisms:
- Estradiol facilitates release in brain areas crucial for memory (e.g., hippocampus), enhances choline uptake, and potentiates receptor sensitivity, thereby supporting cognitive function.
- Progesterone acts on nicotinic acetylcholine receptors, modulating neuronal excitability and neurotransmission.
- Pregnenolone and its sulfate significantly increase levels in the frontal cortex and hippocampus, correlating with neuroprotection and memory enhancement.
- DHEA enhances hippocampal release, supporting mood regulation and cognitive resilience.
- Vitamin D receptors located on cholinergic neurons may influence signaling, though the mechanisms remain under investigation. (See Dr. Stasha Gominak’s insights on vitamin D and acetylcholine)
These interactions suggest a dynamic orchestration by steroid hormones to maintain optimal cholinergic tone, impacting cognition, mood, and autonomic regulation.
Insulin, Glucose, and Acetylcholine Synthesis
This neurotransmitter synthesis’s dependency on acetyl-CoA inherently links it to glucose and insulin metabolism. Glycolysis and the citric acid cycle produce acetyl-CoA—a pathway that cellular insulin sensitivity regulates. Impaired glucose metabolism in insulin resistance and diabetes reduces acetyl-CoA availability, impairing acetylcholine synthesis and cholinergic function.
Dr. Stasha Gominak emphasizes the interdependent relationship among insulin signaling, vagal nerve activity, and production, suggesting that disruptions in these pathways can influence neuroendocrine disorders and metabolic diseases. Optimizing insulin sensitivity and supporting vagal tone may therefore improve cholinergic neurotransmission and overall physiological balance.
Symptoms and Clinical Relevance of Low Acetylcholine
Cholinergic deficiency presents with distinct and wide-ranging symptoms:
- Cognitive impairments such as memory loss, decreased attention, and increased risk of neurodegenerative diseases like Alzheimer’s.
- Autonomic dysfunction manifesting as poor digestion, tachycardia, and impaired glandular secretions.
- Neuromuscular symptoms including muscle weakness and fatigue.
- Emotional disturbances like depression and impaired stress responses.
Given its vital roles, deficiencies disrupt multiple systems and quality of life, underscoring the need for functional cholinergic pathways.
Pantothenic Acid’s Vital Role in Acetylcholine Production
Pantothenic acid (vitamin B5) is the nutritional precursor to coenzyme A (CoA), a critical substrate for acetyl-CoA synthesis. Without adequate pantothenic acid, the body’s capacity to produce acetyl-CoA—and thus ACh—is compromised. This vitamin supports not only neurotransmitter synthesis but also steroid hormone production, energy metabolism, and cellular repair.
Pantothenic acid supplementation shows promise for inflammatory disorders and nerve function, likely by boosting cholinergic signaling. While more robust clinical trials are needed, maintaining sufficient pantothenic acid intake remains essential for neurochemical balance.
Conclusion
ACh serves as a pivotal molecule bridging neuronal communication, autonomic regulation, metabolism, and hormonal modulation. Its biosynthesis intricately depends on nutrient availability and energy metabolism, profoundly impacted by glucose and insulin. Steroidal hormones dynamically influence signaling, shaping brain function and systemic physiology. As experts like Dr. Stasha Gominak emphasize, understanding these relationships enables integrated therapies for neuroendocrine and metabolic health.
Balanced nutrition, hormonal health, and vagal support maintain optimal levels, boosting autonomic function, cognitive resilience, and long-term vitality.
Discover more from The Wellness By Design Project
Subscribe to get the latest posts sent to your email.