Histamine is synonymous with allergic reactions—sneezing, itching, or swelling—but its influence extends far beyond these symptoms. As a biogenic amine, histamine shapes immune responses, hormonal interactions, detoxification pathways, and neurological function. Its complex interplay with mast cells, sex hormones, enzymatic systems, and natural compounds reveals a dynamic molecule requiring nuanced management. This exploration delves into histamine’s multifaceted biology, offering insights into its regulation and strategies for addressing dysregulation.
Recognizing Histamine Dysregulation: Common Symptoms
When histamine levels become dysregulated, such as in cases of histamine intolerance, the body can exhibit a wide array of symptoms that often mimic allergic reactions or other conditions. These arise from histamine’s effects on various systems, including the skin, gastrointestinal tract, respiratory system, and nervous system. Common manifestations include headaches or migraines, which can be triggered by histamine’s vasodilatory effects on blood vessels in the brain. Skin-related issues are prevalent, such as rashes, hives, itching, or flushing, where the face, neck, or chest suddenly becomes warm and red due to histamine-induced vasodilation.
Respiratory symptoms may involve nasal congestion, sneezing, or runny nose, resembling seasonal allergies. In the gastrointestinal system, individuals might experience digestive disturbances like diarrhea, nausea, abdominal pain, or bloating, as histamine influences gut motility and secretion. Neurological and psychological effects can include anxiety, irritability, fatigue, or sleep disturbances, stemming from histamine’s role as a neurotransmitter. Cardiovascular symptoms, such as low blood pressure or irregular heartbeat, and hormonal issues like dysmenorrhea in women, further highlight histamine’s systemic impact. These symptoms vary in intensity and can be exacerbated by dietary histamine intake, hormonal fluctuations, or impaired detoxification pathways, making early recognition crucial for effective management.
Mast Cells: Histamine’s Command Center
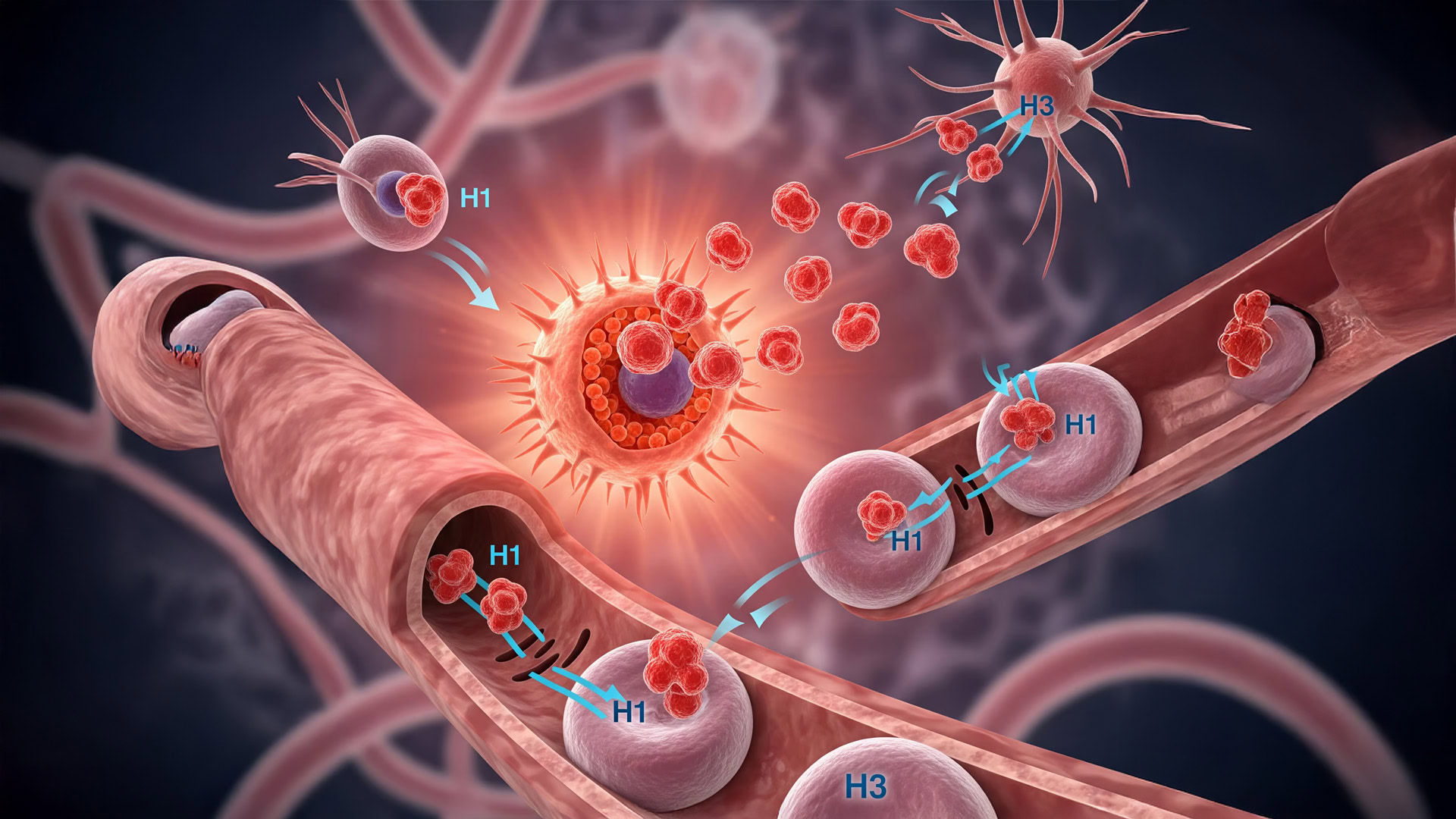
Mast cells, specialized immune cells, serve as histamine’s primary reservoir and release point. Found in tissues exposed to external threats—skin, airways, gastrointestinal tract, and blood vessels—these cells act as sentinels, responding to allergens, pathogens, or physical stress. When triggered, mast cells undergo degranulation, releasing histamine alongside cytokines and lipid mediators to initiate immune responses.
This release sets off a cascade of physiological effects. Histamine binds to four receptor subtypes—H1, H2, H3, and H4—each mediating distinct actions. H1 receptors drive vasodilation and smooth muscle contraction, contributing to allergic symptoms. H2 receptors regulate gastric acid secretion, while H3 and H4 receptors modulate neurotransmission and immune cell activity, respectively. This receptor diversity underscores histamine’s broad influence, from local inflammation to systemic signaling.
Mast cells also amplify immune responses by recruiting other cells, creating a feedback loop that intensifies inflammation. They express receptors for sex hormones, allowing endocrine signals to shape their behavior. Estrogen heightens mast cell reactivity, increasing histamine release, while progesterone often exerts a calming effect. These hormonal interactions explain why histamine-related symptoms may fluctuate across the menstrual cycle or during pregnancy, offering a critical lens for understanding individual variability in allergic and inflammatory responses.
Progesterone: Nature’s Antihistamine
Progesterone, a key sex hormone, counterbalances histamine’s pro-inflammatory effects. Mast cells possess progesterone receptors, and their activation triggers antihistaminic mechanisms. By binding to these receptors, progesterone inhibits mast cell degranulation, reducing the release of histamine and other mediators. This dampening effect helps mitigate the inflammatory cascade driving allergic symptoms.
Beyond suppressing degranulation, progesterone influences gene expression, downregulating the production of histamine and its receptors. This reduces tissue sensitivity to histamine’s effects, offering protection during high-progesterone states, such as the luteal phase of the menstrual cycle or pregnancy. Some evidence suggests progesterone enhances the activity of diamine oxidase (DAO), an enzyme critical for histamine breakdown, particularly in the gut. This multifaceted role positions progesterone as a physiological antihistamine, providing relief from histamine-driven symptoms and highlighting the interplay between endocrine and immune systems.
Detoxifying Histamine: Enzymatic Pathways at Work
Uncontrolled histamine accumulation can lead to chronic inflammation, tissue damage, and systemic symptoms like headaches, digestive issues, or mood disturbances. The body relies on two primary enzymatic pathways to neutralize histamine: diamine oxidase (DAO) and histamine-N-methyltransferase (HNMT). Disruptions in either pathway can result in histamine intolerance, marked by an inability to clear histamine efficiently.
Diamine Oxidase (DAO): The Gut’s Gatekeeper
DAO, predominantly expressed in intestinal epithelial cells, serves as the body’s primary extracellular histamine-degrading enzyme. It catalyzes the oxidative deamination of histamine, converting it into inert compounds before it enters systemic circulation. This process prevents histamine absorbed from food or produced in the gut from triggering widespread effects.
DAO’s effectiveness depends on gut health and nutrient availability. Vitamin B6, vitamin C, copper, and zinc act as cofactors, supporting DAO activity. However, gut dysbiosis, inflammatory bowel conditions, or medications—such as antihypertensives, antidepressants, or antibiotics—can impair DAO function, leading to histamine buildup. Addressing these factors through diet, supplementation, or gut health restoration is essential for maintaining DAO’s protective role.
Histamine-N-Methyltransferase (HNMT): Methylation’s Role
Inside cells, HNMT neutralizes histamine through methylation, attaching a methyl group to histamine to render it inactive. This pathway relies on S-adenosyl methionine (SAMe), a universal methyl donor, and requires nutrients like folate, vitamin B12, vitamin B6, and betaine to sustain methylation cycles.
Genetic variations, such as polymorphisms in the MTHFR or COMT genes, can impair methylation efficiency, increasing susceptibility to histamine overload. Environmental factors, including chronic stress, poor diet, or toxin exposure, further compromise this pathway. Supporting methylation through targeted nutrition and lifestyle adjustments is critical for individuals prone to histamine intolerance, particularly when genetic predispositions are present.
Natural Approaches to Histamine Modulation
For those grappling with histamine intolerance or seeking to optimize immune function, natural compounds offer promising relief. These substances stabilize mast cells, inhibit histamine release, block receptor activity, or enhance detoxification. While not a replacement for medical guidance, they complement holistic strategies to manage histamine levels.
Ginger and Turmeric: Anti-Inflammatory Allies
Ginger, a time-honored remedy, contains bioactive compounds that suppress histamine release from mast cells while exerting broad anti-inflammatory effects. Its versatility makes it a valuable addition to diets aimed at reducing histamine-driven inflammation. Similarly, turmeric’s active compound, curcumin, inhibits mast cell degranulation and mitigates downstream inflammatory responses. Pairing curcumin with black pepper extract enhances its absorption, maximizing therapeutic potential.
Quercetin: Nature’s Mast Cell Stabilizer
Quercetin, a flavonoid abundant in capers, onions, and apples, stabilizes mast cell membranes, reducing histamine synthesis and release. Its antioxidant properties further support its role in calming inflammation, making it a cornerstone of natural histamine management. Incorporating quercetin-rich foods or supplements can provide relief for those with seasonal allergies or histamine sensitivity.
Nettle Leaf and Vitamin C: Gentle Antihistamines
Nettle leaf, often consumed as a tea, acts as a mild antihistamine and anti-inflammatory agent, offering relief from allergic symptoms. Its accessibility and gentle action make it a practical choice for daily use. Vitamin C serves as both a cofactor for DAO and a direct histamine scavenger, reducing circulating levels. Regular intake of vitamin C-rich foods or supplements supports histamine clearance and immune balance.
Bromelain, Probiotics, and Beyond
Bromelain, an enzyme derived from pineapple, reduces inflammation and complements other antihistamine strategies. However, pineapple’s high histamine content may make it unsuitable for sensitive individuals, requiring cautious use. Probiotics, particularly strains that support gut health, enhance DAO activity and immune regulation, creating an environment conducive to histamine clearance. Foods like capers and watercress, rich in antioxidants, may also block histamine effects, providing dietary options for managing symptoms.
A Holistic Approach to Histamine Management
Managing histamine dysregulation requires an integrative approach addressing hormonal, enzymatic, and environmental triggers. Hormonal balance plays a pivotal role, as estrogen can exacerbate histamine release, while progesterone’s stabilizing effects offer relief. Supporting progesterone through lifestyle or medical interventions may help mitigate symptoms, particularly in women with hormone-driven sensitivities.
Optimizing DAO and HNMT pathways is critical. Ensuring adequate intake of vitamins B6, B12, C, folate, and minerals like copper and zinc supports enzymatic function. Addressing gut dysbiosis through probiotics or dietary changes enhances DAO activity, while methylation support through targeted supplementation improves HNMT efficiency. Genetic testing may reveal polymorphisms necessitating personalized nutritional strategies.
Natural compounds like quercetin, ginger, and turmeric provide accessible tools for reducing histamine release and inflammation. Combined with professional guidance, these interventions allow tailored management plans that minimize reliance on pharmaceuticals. By addressing the root causes of histamine dysregulation—hormonal imbalances, enzymatic deficiencies, and environmental triggers—individuals can achieve lasting relief and improved quality of life.
Conclusion: Empowering Histamine Regulation
Histamine’s role transcends its reputation as an allergy trigger, influencing immune, hormonal, and neurological systems. Its release from mast cells, modulated by sex hormones like progesterone, and cleared through sophisticated enzymatic pathways, underscores its complexity. Disruptions in these systems can lead to histamine intolerance, with far-reaching effects on health and well-being.
By understanding the interplay of mast cell activity, hormonal influences, and detoxification pathways, individuals and practitioners can develop targeted strategies. Natural compounds offer gentle, effective support, while nutritional and lifestyle interventions address underlying imbalances. Empowered with this knowledge, those affected by histamine dysregulation can reclaim control, harnessing the body’s innate mechanisms to restore balance and vitality.
Products
Discover more from The Wellness By Design Project
Subscribe to get the latest posts sent to your email.